How to Bill for Concurrent RPM & CCM Codes in a Practice: Part 3
MHA Search
For the latest academic year, we have 170 schools in our MHAOnline.com database and those that advertise with us are labeled “sponsor”. When you click on a sponsoring school or program, or fill out a form to request information from a sponsoring school, we may earn a commission. View our advertising disclosure for more details.
Remote physiological monitoring (RPM) and chronic care management (CCM) codes are increasingly attracting the interest of clinical groups that range from small private practices to large health systems. These codes can provide reimbursement for the provision of care services that complement evaluation and management (E&M) activity for Medicare (and in some states, Medicaid) populations.
This three-part series aims to provide readers with a basic framework to conceptualize the fundamental components of RPM and CCM care provision, and estimate expected patient revenue as well as labor costs in providing the care, using a care team approach to staffing that relies less heavily on the direct interaction with a physician or an advanced that extends the reach of an overseeing physician, nurse practitioner (NP), or physician associate (PA).
In part one of this series, we explored RPM codes and implementation. In part two, we did the same for the CCM codes. In this third and final part of the series, we will touch upon the basics of concurrent billing, and walk through a care team labor costing example.
Readers will benefit from reading parts one and two prior to part three.
RPM Code Refresher
RPM codes center around the use of a technological device, which is used by the patient to collect and transmit one or more variables of biometric data into the electronic health record (EHR) on at least 16 days a month. Both acute and chronic diseases are eligible for RPM program enrollment, so long as the patient is a Medicare (and in some states, Medicaid) beneficiary, and there is an existing established patient-provider relationship. Whether or not a new patient visit by telemedicine is sufficient will vary by state, so local laws should be carefully reviewed prior to any program investment.
After device set-up is billed, ongoing care components can be grouped into data transmission, data review, and patient communication related to the data. Most private payers are not yet reimbursing for these codes, but this may change over time as preventative care continues to demonstrate its cost-effectiveness and its meaningful impact on long-term cost reduction. Reimbursement rates for the RPM codes are reasonable and reflect the relatively more modular approach to RPM care provision.
The lion’s share of the hands-on activity can be performed by clinical staff under the supervision of the billing provider by way of “incident to” billing. CMS has clarified for most (but not all) of the RPM codes that “general supervision” rather than “direct supervision” is permissible for the incident to structure.
This is of great relevance to programmatic design because direct supervision requires the billing provider to be in the same building at the same time as clinical staff when they are performing the work, which can be limiting. General supervision, on the other hand, brings great flexibility by removing this “same building, same time” requirement, so long as everyone is within the same state.
Note that one of the RPM codes (CPT 99457), which is the first 20 minutes of interactive communication with the patient regarding the transmitted data, did not receive explicit CMS clarification on general supervision being sufficient. As such, it may be prudent to assume direct supervision is required for 99457 for the time being; at minimum, it is imperative to consult with an appropriate regulatory and compliance expert for guidance.
CCM Code Refresher
CCM is centered around the concept of the comprehensive care plan and requires the patient to have at least two chronic diseases. CCM codes do not require a technology component, but they do require a number of service components that must first be put into place by the practice before initiation of a CCM program. (More information on the specific requirements can be found in part two of this series). Like RPM, CCM reimbursement is for Medicare (and in some states Medicaid) populations, with few private payers currently reimbursing for these codes.
The management of transition care, emergency room visit follow-up, referral oversight, and communicating information on activity within any of these areas in a prompt manner to all other clinical practices involved with the patient’s care is indeed a helpful area for potential outsourcing of services to a third party. Whether this is financially preferable will depend on a number of factors unique to the practice, such as the price of services, scale and growth estimates of the program population, geographical location, the prevalence of certain diseases, and so forth.
Importantly, the requirement of the patient having 24/7 access to a member of the clinical care team for any acute issues that stem from the chronic diseases being managed, coupled with the requirement of communication directly with the overseeing provider (such as written message communications), must be recognized as a substantial source of provider labor time cost. Even time on-call is still time that has a cost. These components cannot be outsourced at any scale. CMS has clarified it is not sufficient to use a message-taking service and wait until the next business day for a care team member to return the call.
Concurrent Billing and Restrictions
Despite some similarities between RPM and CCM programs, CMS has ruled that the code bodies are complementary; as such, it is indeed permitted to bill one patient for both so long as the criteria for both have been met in full.
Logically, no double-counting of minutes is permitted under any circumstances; if activity minutes are accrued and submitted for one code, consider them ‘used up’ for any others. But beyond the no double-counting rule, restrictions on concurrent billing with RPM and CCM are not excessive. Here is a short list of the more commonly encountered rules on concurrent billing:
- Complex CCM may not be billed in the same period as prolonged E&M activity by the same provider, but simple CCM is permitted to bill concurrently.
- CCM/RPM codes submitted on the same day as an E&M code by the same provider must include an appropriate modifier to indicate shortened service, which subsequently reduces reimbursement for the code. (Since CCM and RPM codes can be billed with a date of service anytime between sufficient activity minute accumulation and the end of the service period, this is easily remedied by submitting CCM/RPM using a different date of service than that of the E&M activity, which has no options other than the date it took place.)
- CCM and RPM activity minutes accrued on a date in which the overseeing provider provided E&M services may not be counted in total accruals for the billing period, except for those specific to initial set-up billing codes for RPM/CCM.
- CCM may not be billed within the same period by any provider as the codes for some end-stage renal disease services (specifically, CPT 90951-90970).
- CCM may not be billed within the same period by the same provider with home health care supervision/hospice care supervision (HCPC G0181-2), but an alternative provider group can submit for reimbursement.
- RPM codes cannot be billed in the same period as continuous glucose monitoring (CPT 95250).
- RPM codes cannot be billed in the same period as blood pressure self-monitoring (CPT 99473-4).
- Payments for patients receiving care who live in certain types of facilities may be ineligible for RPM and CCM codes, depending on the nature of the arrangement and scope of services provided therein. This area is particularly nuanced and should be discussed with a regulatory and compliance expert to assess programmatic feasibility well in advance of any pilot rollout.
- While RPM and CCM (either complex or simple) may be billed concurrently, non-permitted concurrent billing rules from other code sets will still apply to each respective code body, and as always, CMS guidance should be carefully reviewed.
Tracking Labor Cost Using Activity Minute Tracking
It is quite helpful to implement a structure that accurately captures the labor costs of all clinical staff involved in providing RPM/CCM care in addition to the overseeing provider. While the cost of physician or advanced practitioner time is indeed significantly greater than that of non-provider clinical staff, the provider time is a very small proportion of the total activity minutes that will accumulate for billing of these codes.
An ideal structure is one that passively captures this data, by pulling from the activity minutes that must be tracked for billing compliance already. A dedicated database should be built that ties the costs of each staff member (including overhead) to the minutes of activity performed in a matrix fashion.
Even something as simple as a linked spreadsheet on a shared secure server may be sufficient. Ensure that all hardware, software, networks, and policies for permissions access are thoroughly vetted by information security experts, like all digital activity in healthcare.
Particularly at the initial pilot phase, a lower-cost method—even if it does require some manual data tracking at first—can be a prudent choice. This helps to avoid overinvesting should a program fail to reach growth goals, or if managing patients requires more labor minutes than can be provided with current staffing levels at the time.
Starting with clean data capture is crucial as it avoids the need for manual clean-up. Clean data should be relatively straightforward to backload into a future system when the timing makes sense
The operational costing data is crucial to managing, maintaining, or growing the margins of a program. It will show which codes are relatively more profitable with respect to the labor cost, suggesting which bundles are the best to select when aggregating activity for submitting the charges.
It can help to optimize staffing and provide an earlier alert when capacity is being reached with current staffing levels. This data can, over time, provide insight into where technological investment or outsourcing should be explored to further grow the program and its margin.
Adding a dashboard visualization capability to this relatively simple body of data puts key performance indicators in front of decision-makers without manual generation of a report each time. Also, this data can be aggregated to build financial statements that will regularly update if they are interfaced with other key pieces of data.
CMS will continue to release statements that modify the specific details down to a per-code level, whereby even a small change can substantially impact the operating margin of the larger program. Be prepared with the right structure to assess their impact on operations. Indeed, while a model capturing down-to-the-minute labor costs may seem excessively detailed, it will ensure these small changes can be rapidly incorporated and the larger picture impact accurately assessed.
Labor Cost Example Scenario
Here is one example of how activity minutes can be reused in a labor cost calculator for RPM/CCM operations. Fundamentally, a tracking structure is designed to match up who spent how many minutes, on which patient, within which month, regardless of how the behind-the-scenes interfacing is built.
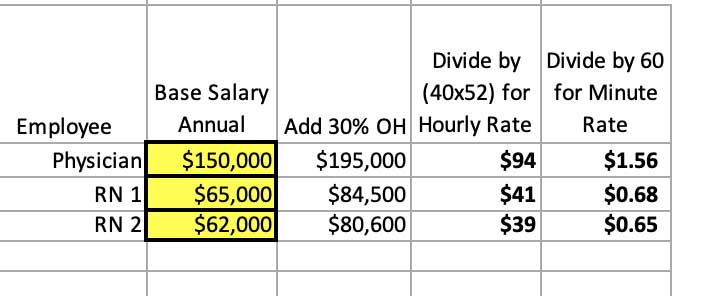
First, there must be defined numbers that represent the fully loaded cost of time for each employee. In this example, we added an additional 30 percent cost on top of their base salary to account for overhead (OH) costs such as paid time off, health insurance benefits, and so on.
On our table, we have our overseeing physician and the two registered nurses costed out. Dividing the fully loaded annual cost by (40 x 52) provides the hourly cost for each. We divide again by 60 for fully loaded cost per minute.
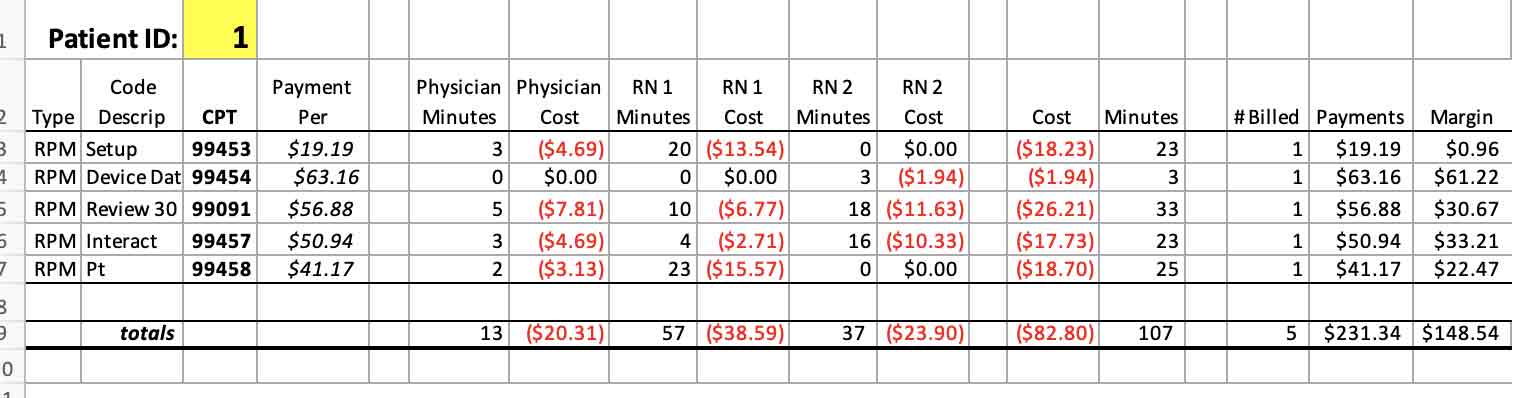
The next table shows the accrued activity minutes for a single patient, broken apart by employee role and associated with their intended bill code. This is a one-month accumulation of a newly enrolled RPM patient.
Note that for purposes of charting, the primal record entry should capture a record of each individual event or interaction using a start and stop time, and not just summary totals by the role as seen here. There must be an intermediary calculation that bundles the minutes appropriately, as well as a mechanism for assigning by code. We will not show this here, but this can be compiled in Excel and linked to other sheets in a number of ways without additional software.
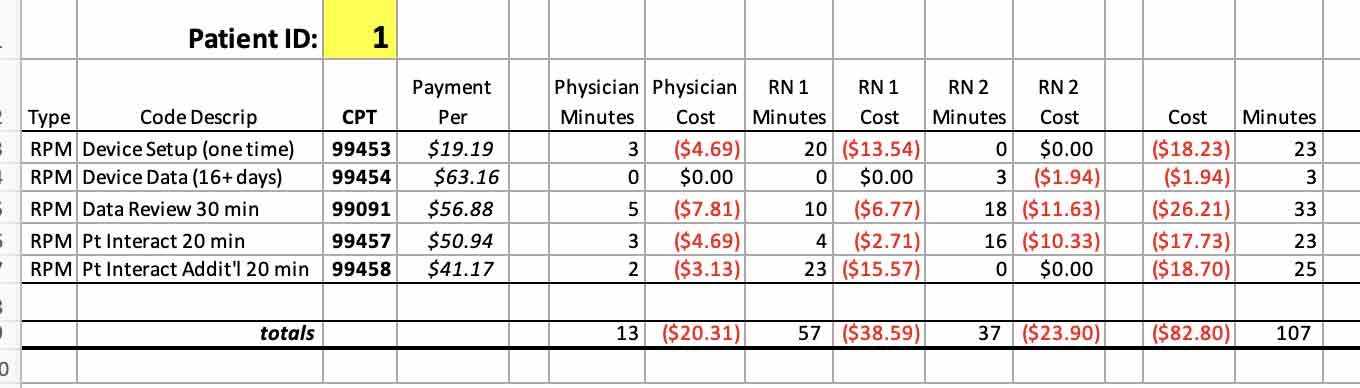
We pull the per-minute fully loaded labor cost from the first sheet, multiply by total minutes per staff member, and we have a good estimate of how much the RPM care for this patient cost in labor time this month.
Recall our example tables from parts one and two of this series, in which the expected annual revenue for a single patient was calculated for an RPM and CCM program. Combine that revenue with the above cost and ensure you are matching the same time periods for each, and you can then calculate a reasonable estimate of operating margin by simply adding on any other appropriate overhead not tied into labor costs already.
That overhead is particularly substantial for the CCM clinical components required to provide the services and relatively less so for RPM (the details behind this are in parts one and two of the series), so it is particularly important for a CCM roll-out to critically examine costs of those services components and to include them on even a rough financial analysis.
There are many software offerings available that can streamline exactly these types of tracking processes and basic calculations therefrom. Some software can perform a small degree of charge review by verifying that accrual thresholds were met for the desired codes. There is even software that can analyze the activity minutes data and suggest the most appropriate (i.e., profitable and compliant) combination of codes to submit for each patient at the month’s end to maximize revenue or margin.
Using login-driven time capture mechanisms can reduce or even eliminate the cost of manually tracking minutes, thereby preventing improper charges, but some users may be resistant to what they may perceive as an overly simplified productivity metric that can be misused by management in assessing performance.
It must also be emphasized that software can only mimic the logic that is built into it by people, who are interpreting CMS rulemaking and releases to the best of their ability and not without error from time to time. CMS guidelines are imperfect, ambiguous, and at times contradictory, and so any changes to them require quick changes to the software and logic —but without causing delays, bugs, glitches, or security breaches of excessively disruptive nature or cost.
Even in the absence of any of the above situations, the adoption of specialized software into a larger clinical operation has an unfortunate tendency to result in redundant data entry somewhere within the workflow for many practices. The cost of manually tracking pilot data may be well less than the cost of investing in the wrong technology solution found out after the fact.
Overall, the most important takeaway is to approach specialized software solutions critically and cautiously, and to consider manually tracking in a more simple spreadsheet at a pilot stage to avoid putting the cart before the horse.
Conclusion: The RPM & CCM Code Series
This RPM/CCM code series is intended to educate clinical leaders and management on some core logistics of implementing RPM and CCM program components at a boots-on-the-ground level.
While the initial set-up can feel overwhelming to managers who are less familiar with the history of these codes, the potential benefit of these programs to a clinical practice can be substantial, not only in terms of financial gain but also improvement of patient population health outcomes.
Ultimately, outcomes-based reimbursement will become a standard metric with payers, and gaining experience with these code bodies now will be particularly valuable in better preparing leadership for the future of care standards.

